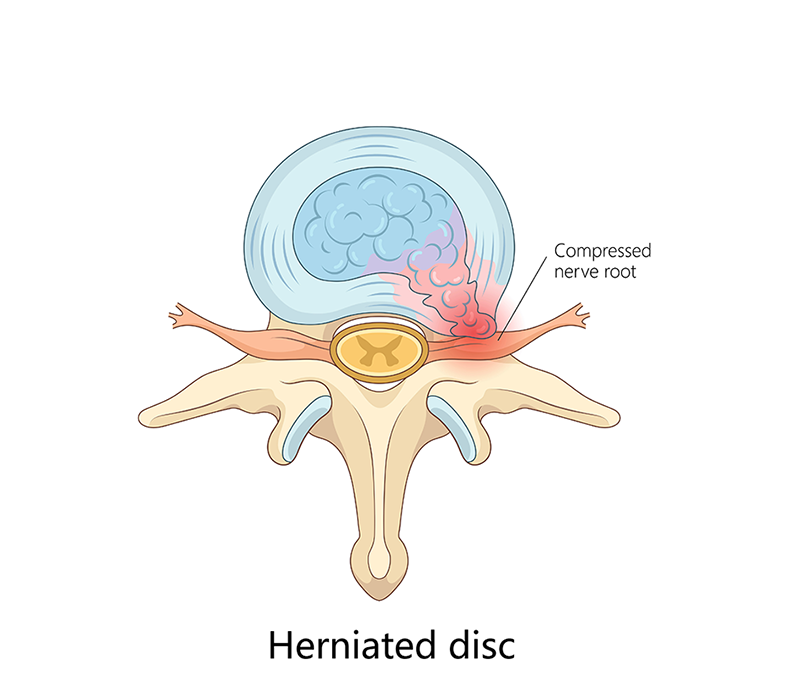
Herniated Disc
A herniated disc occurs when the soft inner gel of disc pushes outward through a tear in the outer layer of the disc. Many people have this condition without being aware of it, as not all herniations cause symptoms. However, if sever enough, this protrusion can press on nerves in the vicinity leading to pain, numbness, or weakness in the area of the body those nerves run to. The most common cause of a herniated disc is from age related wear and tear, also known as disc degeneration. As we age, the discs in our spine are more prone to becoming ruptured or tearing as they begin to become less flexible and lose their shock-absorbing ability. Other common risk factors and triggers include: lifting heavy objects improperly, sudden twisting movements, and trauma.
Overview
A herniated disc occurs when the soft inner material of an intervertebral disc protrudes
through a tear in the outer layer. This can compress nearby nerves, causing pain, numbness,
or weakness. Herniated discs are most common in the lumbar spine (lower back) but can
also occur in the cervical spine (neck).
Types of Herniated Discs
Cervical Herniated Disc: Occurs in the neck, causing neck pain and arm symptoms.
Herniated Disc: Less common; affects the upper/mid-back.
Lumbar Herniated Disc: Most frequent; can cause lower back pain and sciatica.
Causes
Common causes include:
Age-related disc degeneration.
Sudden trauma or injury.
Repetitive lifting, bending, or twisting.
Poor posture over time.
Obesity increasing spinal stress.
Symptoms
Symptoms vary by location and severity:
Sharp or burning back or neck pain.
Radiating pain into arms or legs.
Numbness or tingling.
Muscle weakness.
Difficulty standing or walking.
Diagnosis
Evaluation may include:
Physical Exam: Testing reflexes, strength, and sensation.
MRI: The most useful imaging to visualize herniation.
CT Scan: Provides detail on bone and disc spaces.
X-rays: Help rule out other causes.
Nerve conduction studies: Assess nerve function.
Conservative Treatment
Most herniated discs improve without surgery:
Rest and activity modification.
Nonsteroidal anti-inflammatory drugs (NSAIDs).
Physical therapy exercises.
Epidural steroid injections.
Heat and ice therapy.
Surgical Treatment
Surgery may be considered if symptoms persist or worsen:
Endoscopic discectomy: Removing the herniated portion of the disc.
Partial Laminectomy: Removing part of the bone to relieve pressure.
Recovery varies based on procedure and individual health.
Frequently Asked Questions
Q: Is a herniated disc the same as a bulging disc?
A: No. A bulging disc protrudes without rupture; a herniated disc has inner material escaping.
Q: Can a herniated disc heal on its own?
A: Yes. Many improve with conservative care over weeks to months, however if pain persists surgery may be necessary.
Q: When should I see a doctor?
A: If you experience severe pain, weakness, or loss of bladder/bowel control.
Q: How long does recovery take?
A: Most people feel better within 6-12 week.