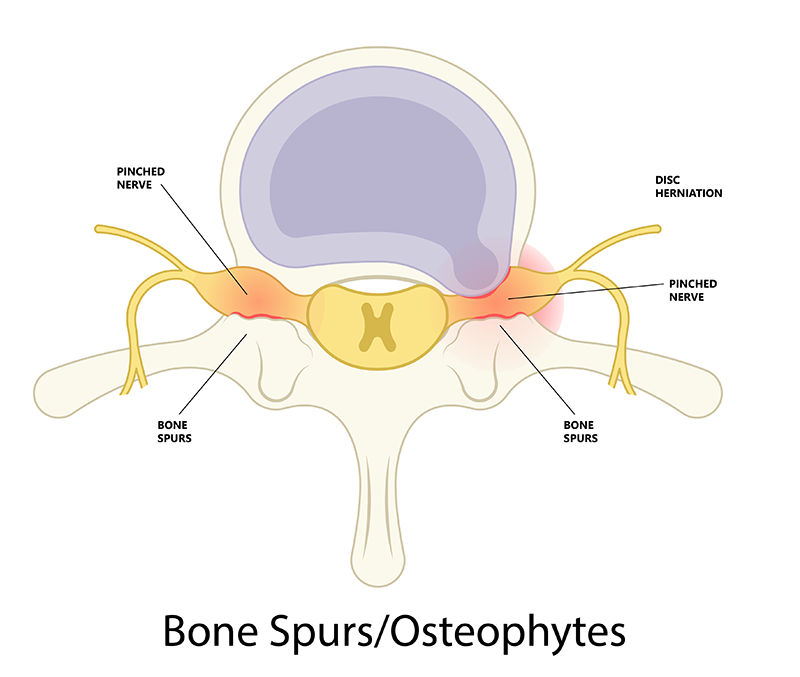
Bone Spurs
Bone spurs, also known as osteophytes, are bony projections that form along the edges of bones. In the context of the spine, bone spurs typically occur on the vertebrae or around the joints as a response to degenerative changes. These bone spurs are the body’s attempt to stabilize a joint that has lost cartilage or height of the disc. However, sometimes, these “repairs” can protrude and crowd nearby nerves. Bone spurs in the spine often accompany spondylosis and are a component of spinal stenosis when they encroach on the spinal canal or intervertebral foramina.
Overview
Bone spurs in the spine, also known as osteophytes, are bony projections that develop along the edges of bones. They often form where bones meet each other—in joints—or on the bones of the spine. While bone spurs themselves are not always painful, they can press on surrounding nerves, tendons, or other structures and cause discomfort or restrict movement.
Types of Bone Spurs
Cervical Spine (Neck) Bone Spurs or Osteophytes
Thoracic Spine (Mid Back) Bone Spurs or Osteophytes
Lumbar Spine (Low Back) Bone Spurs or Osteophytes
Causes
Bone spurs generally develop as the body’s response to:
– Joint damage from osteoarthritis
– Aging-related cartilage degeneration
– Chronic inflammation (e.g., tendinitis)
– Trauma or injury
– Genetic predisposition
– Repetitive stress on bones and joints
Symptoms
Many people have bone spurs without any symptoms. When symptoms occur, they may include:
– Dull or sharp pain near the affected joint
– Swelling
– Stiffness or reduced range of motion
– Numbness or tingling (if nerves are compressed)
– A noticeable hard lump under the skin
Diagnosis
Diagnosis typically involves:
– Physical Examination: Checking joint tenderness, movement, and swelling.
– X-rays: The most common imaging to visualize bone spurs.
– MRI or CT Scans: For detailed images of soft tissues and nerve compression.
– Nerve Conduction Studies: If nerve involvement is suspected.
Conservative Treatment
Most bone spurs can be managed without surgery. Treatment options include:
– Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): To relieve pain and inflammation.
– Physical Therapy: To improve strength, flexibility, and joint function.
– Corticosteroid Injections: Reduce localized inflammation and pain.
– Orthotics or Braces: Help offload stress from the affected joint.
– Activity Modification: Avoiding activities that worsen symptoms.
Surgical Treatment
If conservative measures fail or nerve compression is severe, surgery may be recommended:
– Osteophyte Removal: Surgical excision of the bone spur.
– Joint Replacement: In cases of advanced arthritis.
– Spinal Decompression: If spinal bone spurs compress nerves.
– Arthroscopic Debridement: Minimally invasive removal in joints.
Frequently Asked Questions
Q: Are bone spurs cancerous?
A: No. Bone spurs are benign growths and not related to cancer.
Q: Can bone spurs go away on their own?
A: They do not disappear naturally, but symptoms can improve with treatment.
Q: When should I see a doctor?
A: If you experience persistent pain, numbness, or weakness, consult a healthcare professional.
Q: Do bone spurs always require surgery?
A: No. Most improve with non-surgical treatment.